Recent twin studies have shown novel ways of regenerating a damaged heart
Heart failure affects at least 26 million people worldwide and is responsible for numerous fatal deaths. Due to rise in ageing population, taking care of the heart is becoming a need leading to rise in expenditures. There have been significant advances in therapeutic treatments for the heart and lot of preventive steps are being taken, however, mortality and morbidity is still very high. Very few Treatment options are available and mostly it rests on heart-transplant for the patients who are really at the end stage and progressing towards complete heart failure.
Our body does have an extraordinary capacity to heal itself, for example liver can be regenerated when is damaged, our skin also most of time and one kidney could take over the function for two. Unfortunately, this is not true for most of our vital organs – including the heart. When a human heart is damaged – caused by a disease or an injury – the damage is perpetual. Example, after a heart attack, millions or billions of heart muscle cells can be lost forever. This loss weakens the heart gradually and leads to serious conditions like heart failure, or scars in the heart which can prove fatal. Heart failure usually results when cardiomyocytes (type of cells) become deficient. Unlike newts and salamanders, human adults cannot spontaneously regrow damaged organs such as the heart. In a human embryo or when a baby is growing in the womb, heart cells divide and multiply which helps the heart to grow and develop for nine months. But mammals including humans do not possess the ability to regenerate the heart as they lose this ability subsequently and completely after about a week of being born. Heart muscle cells lose their ability to divide and multiply and hence cannot regenerate. This is true for other human cells too – brain, spinal cord etc. Since these adult cells cannot divide, the human body cannot replace the cells which are damaged or lost and this leads to diseases. Though this is also the reason why there is never a heart tumour – tumours are caused due to uncontrolled growth of cells. If, however, it can be made possible for these cells to divide again, this could lead to “regeneration” of a number of tissues and help to repair an organ.
The only one option which anyone has when suffering from a weak or damaged heart or a heart disease is to receive a heart transplant. This has multitude of aspects which generally affect a transplant from becoming a reality in most patients. Firstly, the heart that is donated by a “donor” has to be a healthy heart before the donor passed away, which means that the heart needs be harvested from young people who have died because of illness or injuries and these conditions have not affected their heart in any way. The prospective recipient patient must match with the donor heart to receive the transplant. This translates into a long wait. As a possible alternative, the potential to be able to create new muscle in the heart through cell division could offer hope to millions with damaged heart. Many procedures have been tried and tested by the scientific community, however, results so far have been ineffective.
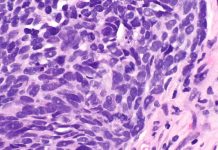
In a new study published in Cell, researchers at University of California, San Francisco, USA have for the first time developed an efficient and stable method in animal models to make adult heart cells (cardiomyocytes) divide and thus potentially repair the damaged portion of the heart1. The authors identified four genes which are involved in cell division (that is cells which multiply on their own). When these genes were combined with genes which cause mature cardiomyocytes to re-enter into a cell cycle, they saw that cells were dividing and reproducing. So, when the function of these four essential genes was enhanced, the heart tissue showed regeneration. After heart failure in a patient, this combination improves heart function. Cardiomyocytes exhibited 15-20 percent division in the current study (compared to 1 percent in earlier studies) cementing reliability and efficiency of this study. This study could technically be extended tp other organs because these four genes are a common feature. This is a very relevant work because any study on the heart is firstly very complicated and secondly the delivery of genes has to be done with caution so as not to cause any tumours in the body. This work could turn into a very powerful approach for regenerating the heart and also other organs.
Another study by Stem Cell Institute, University of Cambridge, UK, has developed an innovative way to repair heart tissue such that a donor would not be required at all2. They have used stem cells to grow live patches of “heart muscle” in the laboratory which are only 2.5 square centimetres but they look like a powerful potential tool to treat patients who have heart failure. These patches have a bright prospective of getting naturally assimilated into a patient’s heart i.e. it’s a “fully functional” tissue which beats and contracts just like a normal heart muscle. An earlier approach of injecting stem cells into the body to repair the heart has been unsuccessful because stem cells did not stay in the heart muscle but instead got lost in the blood. The current patch is a “live” and “beating” heart tissue that can be attached to an organ (in this case the heart) and thus any damage could be repaired. Such patches could be grown as and when there is a demand for a patient. This would essentially surpass the need to wait for a matching donor. These patches could also be grown using the heart patient’s own cells eliminating the risks that are involved in organ transplant. Assimilating the patch into a damaged heart is an invasive procedure and requires correct electrical impulses for making the heart beat well-integrated with a patch. But the risks involved in this kind of procedure are better that a total heart transplant which is much more invasive. The team is getting ready for animal trials and clinical trials within 5 years before this could be used widely for heart patients.
***
{You may read the original research paper by clicking the DOI link given below in the list of cited source(s)}
Source(s)
1. Mohamed et al. 2018,. Regulation of Cell Cycle to Stimulate Adult Cardiomyocyte Proliferation and Cardiac Regeneration. Cell. https://doi.org/10.1016/j.cell.2018.02.014
2. University of Cambridge 2018. Patching up a broken heart. http://www.cam.ac.uk/research/features/patching-up-a-broken-heart. [Accessed May 1 2018]