Several new strains of the virus have emerged since the pandemic began. New variants were reported as early as February 2020. The current variant that has brought the UK to standstill this Christmas is said to be 70% more infectious. In view of emerging strains, will several vaccines being developed worldwide still be effective enough against the new variants as well? ‘Neutralising Antibody’ approach targeting the virus seems to offer a hopeful option in this current climate of uncertainty. The status is that eight neutralizing antibodies against SARS-CoV-2 are currently undergoing clinical trials, including trials of ‘antibody cocktails’ aimed at overcoming possibility of the virus developing resistance to a single neutralizing antibody by accumulating spontaneous mutations.
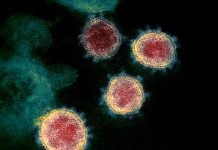
The SARS-CoV-2 virus responsible for COVID-19 pandemic belong to the betacoronavirus genus in the coronaviridae family of viruses. This virus has a positive-sense RNA genome, meaning the single strand RNA act as messenger RNA while directly translating into viral proteins in the host. The genome of SARS-CoV-2 encodes four structural proteins {spike (S), envelope (E), membrane (M), and nucleocapsid (N)} and 16 non-structural proteins. While the structural proteins play role in receptor recognition on the host cell, membrane fusion, and subsequent viral entry; the non-structural proteins (NSPs) play crucial role in replicative functions such as RNA polymerization by the RNA-dependent RNA polymerase (RdRp, NSP12).
Significantly, RNA virus polymerases do not have proofreading nuclease activity, meaning there is no mechanism available to check for the errors during transcription or replication. Therefore, viruses of this family display extremely high rates of variation or mutation. This drives their genome variability and evolution thereby providing them extreme level of adaptability and helping the virus escape the immunity of the host and developing resistance against the vaccines (1,2,3). Obviously, it has always been nature of RNA viruses, including coronaviruses to undergo mutations in their genome at extremely high rates all the time due to the reasons mentioned above. These replication errors that help the virus overcome negative selection pressure, lead to adaptation of the virus. In the long run, more the error rate, more the adaptation. Yet, COVID-19 is the first documented coronavirus pandemic in history. It is the fifth documented pandemic since the 1918’s Spanish flu; all of the earlier four documented pandemics were caused by flu viruses (4).
Apparently, human coronaviruses have been building up mutations and adapting in the last 50 years. There have been several epidemics since 1966, when the first epidemic episode was recorded. The first lethal human coronaviruses epidemic was in 2002 in Guangdong Province, China that was caused by the variant SARS-CoV followed by 2012 epidemic in Saudi Arabia by the variant MERS-CoV. The current episode caused due to SARS-CoV-2 variant started in December 2019 in Wuhan, China, and subsequently spread worldwide becoming the first coronavirus pandemic leading to COVID-19 disease. Now, there are several sub-variants spread across different continents. SARS-CoV-2 has also shown inter-species transmission between humans and animals and back to humans(5).
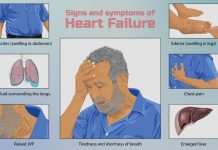
The vaccine development against human coronavirus did start after 2002 epidemic. Several vaccines against SARS-CoV and MERS-CoV were developed and underwent preclinical trials but few entered human trials. None of them received FDA approval though (6). These efforts came handy in vaccine development against SARS-CoV-2 through usage of existing preclinical data including those relating to vaccine design performed during development of vaccine candidates for SARS-CoV and MERS-CoV (7). At this point of time, there are several vaccines against SARS-CoV-2 at a very advanced stage; few have already been approved as EUA (Emergency Use Authorization). About half a million high-risk people in the UK have already received Pfizer’s mRNA vaccine. And, here comes the report of newly emerged, highly infectious strain (or, sub-strain) of SARS-CoV-2 in the UK this Christmas time. Temporarily named VUI-202012/01 or B117, this variant has 17 mutations including one in spike protein. More infectious doesn’t necessarily mean that the virus has become more dangerous for humans. Naturally, one wonders if these vaccines will still be effective enough against the new variants as well. It is argued that a single mutation in the spike should not make vaccines (‘spike region’ targeting) vaccine ineffective but as the mutations accumulate over time, vaccines may need fine tuning to accommodate antigenic drift (8,9)
Antibody approach: renewed emphasis on neutralising antibodies may be imperative
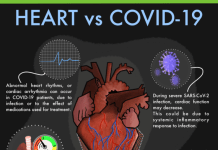
It is in this background that the ‘antibody approach’ (involving ‘neutralizing antibodies against SARS-CoV-2 virus‘ and ‘therapeutic antibodies against COVID-19-associated hyperinflammation’) gains significance. Neutralizing antibodies against SARS-CoV-2 virus and its variants may serve as a ‘ready to use’ passive immunity tool.
The neutralising antibodies target the viruses directly in the host and can provide quick protection especially against any newly emerged variants. This route has not shown much progress yet but has the potential to address the problem of antigenic drift and possible vaccine mismatch presented by the fast-mutating and evolving SARS-CoV-2 virus. As on 28 July 2020, eight neutralizing antibodies against SARS-CoV-2 virus (namely LY-CoV555, JS016, REGN-COV2, TY027, BRII-196, BRII-198, CT-P59, and SCTA01) were undergoing clinical evaluation. Of these neutralising antibodies, LY-CoV555 is monoclonal antibody (mAb). VIR-7831, LY-CoV016, BGB-DXP593, REGN-COV2, and CT-P59 are other monoclonal antibodies being tried as neutralising antibodies. Antibody cocktails can overcome any possible resistance developed against a single neutralising antibody, hence cocktails such as REGN-COV2, AZD7442, and COVI-SHIELD also are undergoing clinical trials. However, strains may gradually develop resistance to cocktails as well. Further, there may be risk of antibody-dependent enhancement (ADE) due to antibodies that only bind to the virus and are incapable of neutralising them, thereby worsening disease progression (10,11). A continuum of innovative research work is needed to address these issues.
***
Related article: COVID-19: ‘Neutralising Antibody’ Trials Begins in the UK
***
References:
- Elena S and Sanjuán R., 2005. Adaptive Value of High Mutation Rates of RNA Viruses: Separating Causes from Consequences. ASM Journal of Virology. DOI: https://doi.org/10.1128/JVI.79.18.11555-11558.2005
- Bębenek A., and Ziuzia-Graczyk I., 2018. Fidelity of DNA replication—a matter of proofreading. Current Genetics. 2018; 64(5): 985–996. DOI: https://doi.org/10.1007/s00294-018-0820-1
- Pachetti M., Marini B., et al., 2020. Emerging SARS-CoV-2 mutation hot spots include a novel RNA-dependent-RNA polymerase variant. Journal of Translational Medicine volume 18, Article number: 179 (2020). Published: 22 April 2020. DOI: https://doi.org/10.1186/s12967-020-02344-6
- Liu Y., Kuo R., and Shih H., 2020. COVID-19: The first documented coronavirus pandemic in history. Biomedical Journal. Volume 43, Issue 4, August 2020, Pages 328-333. DOI: https://doi.org/10.1016/j.bj.2020.04.007
- Munnink B., Sikkema R., et al., 2020. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science 10 Nov 2020: eabe5901. DOI: https://doi.org/10.1126/science.abe5901
- Li Y., Chi W., et al., 2020. Coronavirus vaccine development: from SARS and MERS to COVID-19. Journal of Biomedical Science volume 27, Article number: 104 (2020). Published: 20 December 2020. DOI: https://doi.org/10.1186/s12929-020-00695-2
- Krammer F., 2020. SARS-CoV-2 vaccines in development. Nature volume 586, pages516–527(2020). Published: 23 September 2020. DOI: https://doi.org/10.1038/s41586-020-2798-3
- Koyama T., Weeraratne D., et al., 2020. Emergence of Drift Variants That May Affect COVID-19 Vaccine Development and Antibody Treatment. Pathogens 2020, 9(5), 324; DOI: https://doi.org/10.3390/pathogens9050324
- BMJ 2020. News Briefing. Covid-19: New coronavirus variant is identified in UK. Published 16 December 2020. DOI: https://doi.org/10.1136/bmj.m4857
- Renn A., Fu Y., et al., 2020. Fruitful Neutralizing Antibody Pipeline Brings Hope To Defeat SARS-Cov-2. Trends in Pharmacological Sciences. Volume 41, Issue 11, November 2020, Pages 815-829. DOI: https://doi.org/10.1016/j.tips.2020.07.004
- Tuccori M., Ferraro S., et al., 2020. Anti-SARS-CoV-2 neutralizing monoclonal antibodies: clinical pipeline. mAbs Volume 12, 2020 – Issue 1. Published online:15 Dec 2020. DOI: https://doi.org/10.1080/19420862.2020.1854149
***